Guest blog written by Peter Harrington
When he started his blog series on crisis leadership on these pages, Matt Andrews asked: can public leaders navigate high winds and big waves in little boats? We could add to that question: how do you build the boat when you are already at sea and the storm is raging?
For most governments, the mechanisms to deal with this crisis did not exist, and existing ones were not designed for it. As a result, much of the response is being improvised in the middle of a hurricane, and more recent blog posts on Liberia and Bahrain have explored this.
This challenge gives rise to a very common pattern: crisis responders will focus on the problems that have to be solved right now. It is a natural way to go about the job; prioritise what is urgent and solve the problem, then move on to the next. But anyone will familiar with the so-called Eisenhower matrix (‘Urgent versus Important’ 2×2 shown below) will know that we ignore ‘important but not urgent’ issues at our peril.
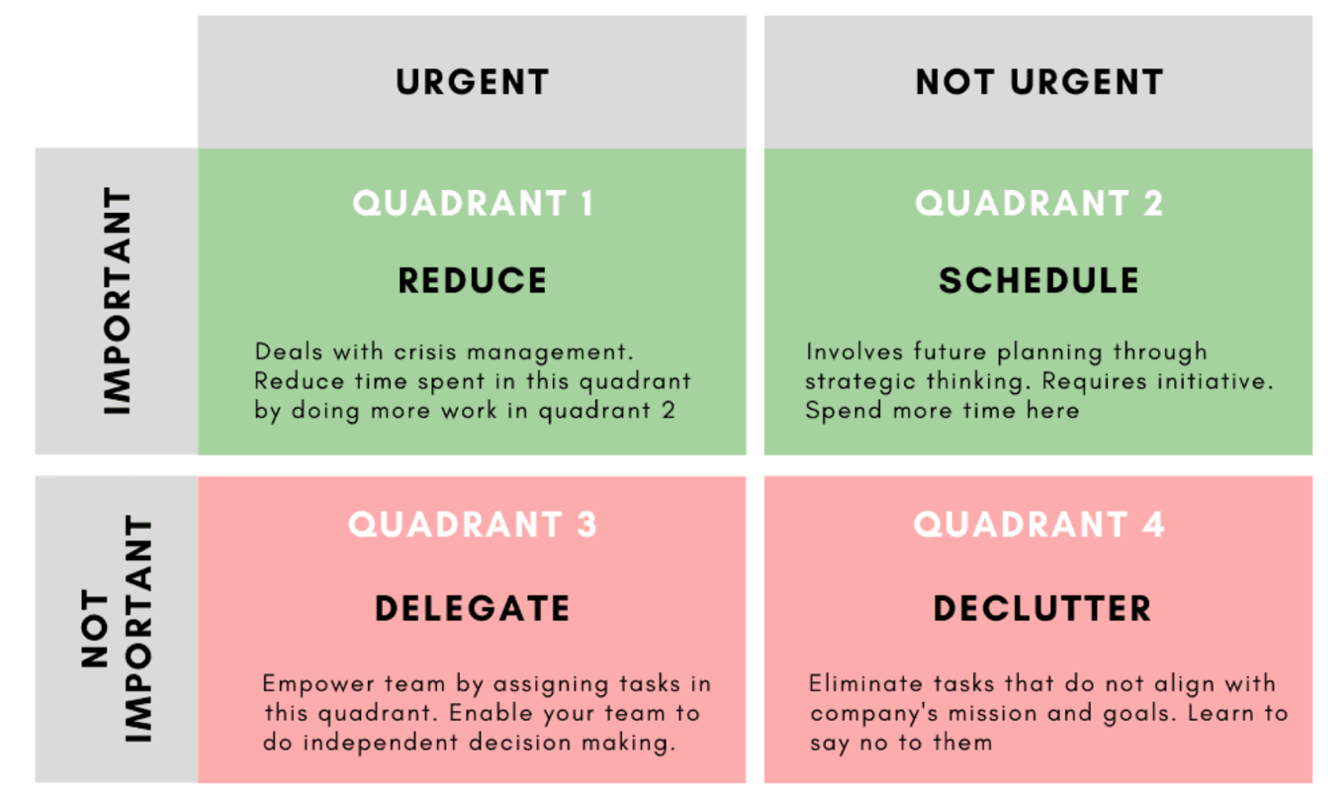
Source: Vinita Bansal’s excellent Techtello article on ‘How to Prioritise and Master Productivity’
The current crisis is no different, and this post is dedicated to the problems which will become critical in the next few weeks and months as the crisis evolves, and which must be planned for (those in quadrant 2 of the matrix and need to be scheduled for action through strategic thinking NOW). Leaders need to make sure they put in place resources to tackle these ‘tomorrow problems’.
COVID-19 is impacting every sector. But for simplicity’s sake, I am going to focus on the two main, broad dimensions of the crisis: the medical (or public health) side in this blog post, and the economic side in the next post. These two dimensions are intimately connected – what happens in one, including the policies implemented, profoundly affects the other. It’s vital to consider how these interdependencies will play out as the crisis evolves, and some countries are doing that already. But forward planning will be especially important in developing and transitional countries which have yet to bear the full brunt of the pandemic.
The medical response: Sword vs scalpel
On the medical side, countries are at different stages of the crisis. The focus so far has been to seek to ‘flatten’ and spread out the transmission curve. This uses social distancing and lockdown to prevent an exponential spike in cases which would exceed the healthcare system capacity, thus buying time and enabling the system to adapt and cope. This is illustrated in the well-known figure below:
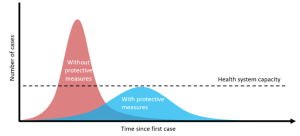
The red curve is the nightmare scenario, as seen tragically in Italy, where hospitals are overwhelmed and terrible clinical choices have to be made. The blue scenario, supposedly, is manageable and achieved by behaviour change – getting people to stay separated through protective measures like lockdown. Such measures are a crude weapon: like a sword being swung at the pandemic, to make the blue scenario more likely. It makes sense that the focus has been on the urgent thing: stop the spike. But there are two big questions hanging over the response: how effective will the sword be in your country? And even if they work, how do you get from the peak to zero? The first question is especially pressing for developing countries. The later question matters for everyone. Let’s start with the latter.
There are well established methods for shutting down an epidemic before it becomes a pandemic. They consist of three key ingredients:
- Testing – to see who has the virus
- Contact tracing – to find everyone who a positive tested case has been in contact with
- Quarantine – of all contacts for the full incubation time, to stop the transmission chain.
This approach is much more precise, like a scalpel instead of a sword. It involves people (an army of health workers) meticulously tracking down each line of the disease and shutting it off. In the early spread of COVID-19 we saw various countries adopt this tactic at first. The reason this approach – which has been urged consistently by the WHO – was replaced by crude lockdowns is because the virus got ahead of the trackers in many countries. Whether or not that was inevitable or not is a debate for another day. What matters is that for countries’ who have chosen lockdown, their only hope of exit and of economic recovery is the scalpel.
The world is currently watching Hubei and South Korea very closely. As the two locations furthest down the road of their COVID-19 epidemic they hold lessons for others on how to exit from lockdown successfully. At the moment there is good reason to believe that their approaches – which rely heavily on testing, tracing, quarantine and border control measures in various combinations – are working. This mirrors the experience from Ebola in West Africa. Once the curve had peaked, getting to zero cases was all about detective work. Although COVID-19 is much more contagious than Ebola and can transmit without symptoms, there is still widespread consensus that these methods are the best hope. As other OECD countries contemplate the gradual easing of restrictions, some combination of these methods will be needed.
Right now leaders are understandably focused on their Urgent pile. But it is critical to start planning and preparing for this detective phase of the crisis so that in 1-3 months time – whatever the shape the curve in a given country turns out to be (and it will probably be somewhere in between the red and the blue) – the country is ready to pivot its approach. The biggest issue at this moment is widespread availability of accurate testing. But if you are a public leader, ask yourself if you are ready to swap the sword for the scalpel:
- Is my country preparing now for later, crucial phases of the medical response?
- What are our strategies to get sufficient testing in place? Where will we get tests?
- Are we preparing to do contact tracing and to enforce quarantine on a large enough scale?
Although urgent ‘today problems’ will consume most resources, national and sub-national responses need to allocate resources now to plan for these ‘tomorrow problems’. The crisis management snowflake can accommodate a ‘Plan-Ahead team’ – as McKinsey calls it – to be looking at these issues. And other teams can and should look even further ahead medically, to the psycho-social and mental health problems which are going to ensue six months from now.
What about the other question? Will the sword work in all countries? The wave of lockdowns across the world has been astonishing and the uniformity of response begs the question of whether isomorphic mimicry is at play. There are several reasons to think that lockdown may not be the most effective approach in many developing countries. First, in some places the dashed line in the figure above representing health system capacity is so low that any hope of keeping the curve beneath it is impossible. Second, urban housing situations in many places – from Kibera to Kolkata – make social distancing a fantasy. Third, in developing countries people do not access food or essential cooking fuel in supermarkets which can be easily controlled. And outside rich countries only a tiny fraction of economic activity can shift onto Zoom and into home offices. These issues, and sensible alternatives, are brilliantly outlined here by W. Gyude Moore, a former Liberian government minister.
For many countries, the scalpel might actually be the best, or only option, or at least more nuanced social distancing measures combined with precision measures. Partly because the sword won’t work, and partly because – as Ricardo Hausmann explains – many countries simply don’t have the fiscal space to deal with the ‘sword wounds’ caused by lockdown. The point is that it depends on the economic, social, political, cultural context, and there’s not enough sign yet that measures are being truly tailored to context. Finally, lest anyone think poor countries can’t do testing, contact tracing and quarantine, remember that in 2014 three of the world’s poorest countries – Sierra Leone, Liberia and Guinea – did it with volunteers armed with clipboards and good risk communications.
The economic response: a great balancing act
COVID-19 will affect every economy in the world, even if a country never has a case of the virus. Global supply and demand have already plummeted, and will lead into a global recession. But much of the economic damage will be self-inflicted, ‘sword wounds’ resulting from the lockdowns which lead to business closures, job losses, loan defaults and halted investment. The public health crisis and the economic crisis are closely intertwined. Measures to mitigate one affect and can undermine the other. Leaders need to pay careful attention to these interdependencies.
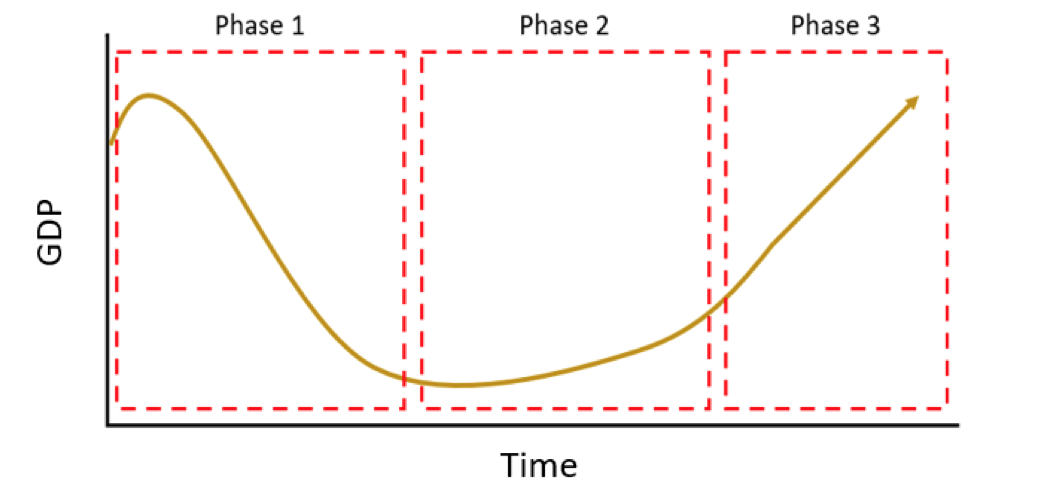
As Jonathan Said, head of Inclusive Growth at the Tony Blair Institute for Global Change explained to me, economies will probably go through three broad phases during this crisis, shown in the stylised figure below:
- Phase One – Shock: In the first phase the economy goes rapidly into recession. Where lockdown policies and extreme containment measures are implemented, the shock to supply as businesses close, and the shock to demand as consumers shelter at home, causes the real economy to contract dramatically. GDP growth rates will turn negative. During Ebola the Liberian economy went from 6% GDP growth to -10%. We are watching this happen in dozens of economies around the world in real time.
- Phase Two – Stabilisation: The Phase 1 contraction in the economy will continue until it approaches a new, low equilibrium where decline in growth will bottom out. The timing and level will be determined by the precise mix of public health policies (e.g. length of lockdown, border controls), the mix of stimulus policies, and the point at which supply cannot fall any further. Depending on the stimulus measures, public health policies and the strength of the real economy, growth will eventually start to recover from zero growth to low growth (1-3%).
- Phase Three: Recovery and reform: In this third phase, the economy theoretically picks up momentum and growth progresses towards previous rates. The timing of this phase depends largely on measures taken in Phase 1 and 2 and the impacts and condition of key sectors. This phase also offers an opportunity for economic disruption and transformation – to make inefficient sectors more efficient, and stimulate new sectors.
The main aim of measures taken in Phase 1 is to cushion the shock as much as possible. The shock is coming from the contraction in the world economy, contraction in the national economy due to changes in behaviour and sentiment, and from a country’s public health measures like lockdown and enforced business closures.
What’s in the Urgent pile? Every economy needs some form of stimulus package to protect businesses and households. But these measures also interact with, and bolster or undermine the counter-epidemic measures. In developing countries, poor and vulnerable populations need cash transfers and possibly food distribution to comply with and survive health policies like lockdown and social distancing. If people cannot stay at home without starving, they cannot follow restrictions and the epidemic will accelerate.
We are seeing many governments struggle with this balance, closing food businesses and impacting food supply chains without sufficient planning. These are quickly becoming binding constraints on an effective medical response.
Rapid steps are needed to keep food markets and essential supply chains open, especially for access to food and cooking fuel. Key workers and suppliers need support to keep markets, ports, transport and utilities operating, but able to accommodate social distancing measures. Businesses forced to close either due to the recession or health policies need help to prevent insolvency through government backed loans and/or insurance policies. In the case of small and micro informal businesses, the lifeline may need to come via social protection-style cash transfers.
The mechanisms in developing countries, with high rates of informality, need to look different to those in OECD countries. Direct cash transfers are much more important in the former. In rural areas, CSOs and village saving schemes may be vehicles for distribution. Mobile money systems should be used where possible.
Given all this, Covid-19 is leaving a large hole in government revenues which needs to be plugged urgently. As Hausmann makes clear, a country’s fiscal space will determine the scale of funding available for stimulus. Most developing countries will have limited capacity to borrow, so will need direct support from the international community. This throws into even further question whether lockdown, which inflicts so much damage on an economy, is the right approach for all countries.
The other aim of the measures taken in the first, shock phase is to make the phase 2 as short as possible, and hasten the transition in to phase 3. Although much will depend on the world economy, the more a country’s recession is V-shaped rather than U-shaped, the better. And here, everything comes down to what happens with COVID-19 within its borders. Exit from the recession hinges on exit from the epidemic; but exiting from the epidemic hinges on getting the economic measures right.
Much has been written about the balance between balancing the impact of the virus itself versus the impact of economic measures, but it is not simply a trade-off. They have to work together, and planning ahead is the only way to do it.
Plan-Ahead teams also need to be looking at the future stages of the economic crisis. While the Urgent pile above remains urgent, on the important pile are issues like the agricultural harvest and planting seasons, financial sector collapse due to loan defaults, and identifying the public works and policies that will help kickstart economic activity and key sectors. Longer term problems include investment promotion, while a smart industrial strategy can target inefficient or indebted sectors, and nurture new sectors to flourish in a recovery.
Leaders need to ask themselves:
- Are our immediate economic measures going to be a binding constraint to the medical response?
- Are we planning sufficiently for kickstarting the economy?
- Are we planning for opportunities for economic transformation?
Epilogue
The medical and economic dimensions of COVID-19 are deeply interconnected, and responses to one can be a binding constraint to the other. Protective medical responses are causing massive economic problems, and policies to relieve those economic problems can, in turn, strengthen or undermine the medical response. This interdependence is the main challenge facing countries today, and will become even more important. Blunt protective measures may not work for all countries, and where used they will need to give way to more precision tools as the crisis evolves. If governments fail to plan now for this evolution, and for problems down the line, they risk getting trapped in a cycle of outbreaks and economic collapse which will affect millions of lives.
Peter Harrington is a principal at Oxford Policy Management and a former BSC Fellow.
